What is anemia?
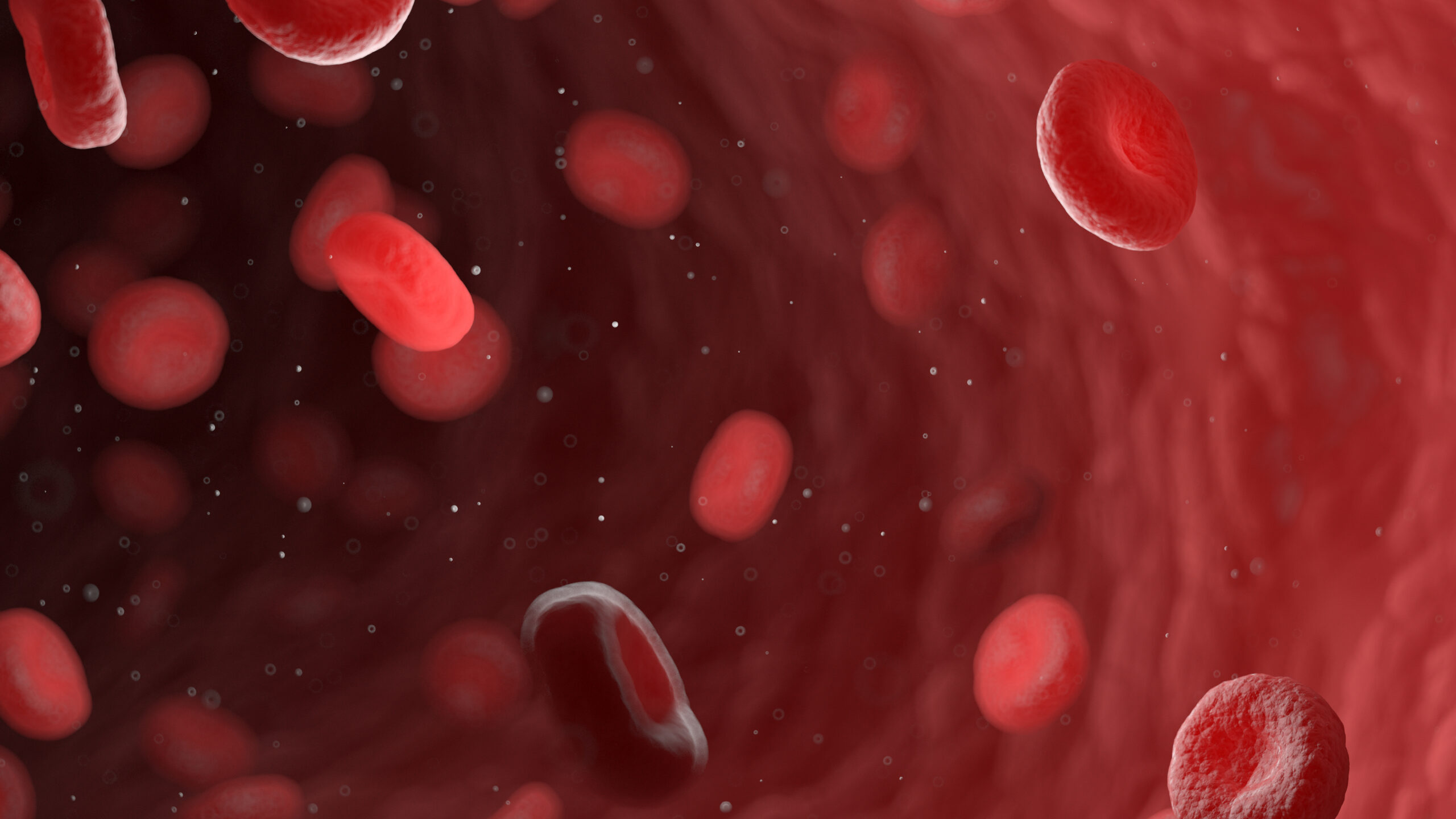
Anemia is a medical condition characterized by a decrease in the number of red blood cells (RBCs) or a reduction in the hemoglobin concentration within the red blood cells. Hemoglobin is a protein responsible for carrying oxygen from the lungs to the rest of the body. A low hemoglobin level or reduced RBC count can lead to decreased oxygen delivery to tissues and organs, resulting in fatigue, weakness, shortness of breath, and other symptoms.
Anemia can be classified into different types based on the underlying cause or the size and appearance of red blood cells. Diagnosis typically involves blood tests to assess red blood cell count, hemoglobin concentration, and other related parameters. Treatment depends on the cause and severity of anemia and may include dietary changes, supplementation, or medical interventions.
How exactly does anemia occur?
Anemia occurs when there is an imbalance in the body’s production, destruction, or loss of red blood cells (RBCs). This can happen through various mechanisms, depending on the underlying cause:
- Blood loss: Acute or chronic bleeding can result in the loss of RBCs. This can be due to trauma, surgery, gastrointestinal bleeding, heavy menstrual periods, or other causes. When blood loss is significant or persistent, the body may not be able to produce new RBCs fast enough to replace the ones that are lost, leading to anemia.
- Decreased red blood cell production: The body may not produce enough RBCs due to several reasons, such as:
- Nutritional deficiencies: Iron, vitamin B12, and folic acid are essential nutrients for the production of RBCs and hemoglobin. A deficiency in any of these nutrients can impair the production of RBCs, leading to anemia.
- Bone marrow disorders: The bone marrow is responsible for producing RBCs. Conditions that affect the bone marrow, such as leukemia, myelodysplastic syndromes, or bone marrow damage from radiation or chemotherapy, can decrease RBC production.
- Chronic diseases: Some chronic diseases, such as kidney disease, cancer, or autoimmune diseases, can interfere with the production of RBCs or the hormone erythropoietin, which stimulates RBC production.
- Genetic conditions: Inherited conditions like thalassemia or aplastic anemia can cause the body to produce fewer or abnormal RBCs, leading to anemia.
- Increased red blood cell destruction: In certain conditions, the body destroys RBCs more quickly than it can produce them. This can be due to:
- Hemolytic anemia: This occurs when RBCs are destroyed prematurely. It can be caused by autoimmune diseases, certain infections, genetic disorders, or certain medications.
- Sickle cell anemia: This is a genetic disorder in which RBCs have an abnormal shape, causing them to break down more easily and leading to anemia.
In all these cases, the end result is a reduced number of functional RBCs or a decreased hemoglobin concentration, which impairs the body’s ability to deliver oxygen to tissues and organs.
What symptoms do patients experience with anemia?
The symptoms of anemia can vary depending on the severity, duration, and underlying cause of the condition. Some people with mild anemia may not experience any symptoms, while others with more severe anemia may have noticeable signs. Common symptoms of anemia include:
- Fatigue or weakness: This is a result of reduced oxygen delivery to tissues and organs, making it harder for the body to produce energy.
- Shortness of breath: With less oxygen-carrying capacity, the body needs to breathe more rapidly to meet its oxygen demands, leading to shortness of breath.
- Paleness or pallor: This is particularly noticeable in the skin, nail beds, and mucous membranes, such as the gums and inner eyelids, due to the reduced concentration of oxygen-carrying hemoglobin in the blood.
- Dizziness or lightheadedness: Insufficient oxygen supply to the brain can cause dizziness or lightheadedness, particularly when standing up or exerting oneself.
- Rapid or irregular heartbeat: The heart may need to pump blood more quickly to compensate for the reduced oxygen-carrying capacity, leading to an increased heart rate or irregular heartbeat.
- Cold hands and feet: Reduced blood flow and oxygen supply to the extremities can cause cold hands and feet.
- Headaches: Insufficient oxygen supply to the brain may result in headaches.
- Chest pain or angina: In severe cases, the heart muscle may not receive enough oxygen, causing chest pain.
- Cognitive or concentration problems: A lack of oxygen in the brain can affect cognitive function, leading to difficulty concentrating or problems with memory.
In addition to these general symptoms, some types of anemia may have specific symptoms related to the underlying cause, such as jaundice in hemolytic anemia or neurological symptoms in vitamin B12 deficiency anemia. If you suspect you have anemia or are experiencing any of these symptoms, it is essential to consult a healthcare professional for a proper evaluation and diagnosis.
How is anemia diagnosed?
Anemia is typically diagnosed through a series of blood tests and a thorough medical history and physical examination. Blood tests are crucial to determine the presence, type, and severity of anemia, as well as to identify possible underlying causes. Common blood tests for diagnosing anemia include:
- Complete blood count (CBC): This test provides information about various components of your blood, such as the red blood cell (RBC) count, hemoglobin concentration, hematocrit (the percentage of blood volume occupied by RBCs), and other parameters like mean corpuscular volume (MCV) and red cell distribution width (RDW). Abnormal values in these parameters can indicate anemia and provide clues about its type.
- Reticulocyte count: Reticulocytes are immature RBCs. A reticulocyte count helps assess the bone marrow’s response to anemia and can help determine if the anemia is due to decreased RBC production or increased RBC destruction.
- Peripheral blood smear: A sample of your blood is examined under a microscope to evaluate the shape, size, and appearance of RBCs, which can provide information about the type of anemia and possible causes.
- Iron studies: These tests measure levels of iron, ferritin (a protein that stores iron), and transferrin (a protein that transports iron) in the blood, which can help determine if anemia is due to iron deficiency or another cause.
- Vitamin B12 and folate levels: These tests measure the levels of vitamin B12 and folate in your blood, which can help identify anemia caused by deficiencies in these nutrients.
- Hemoglobin electrophoresis: This test is used to identify abnormal hemoglobin variants, such as those found in sickle cell anemia or thalassemia.
Depending on the results of these initial tests and the suspected cause of anemia, additional tests may be necessary to confirm the diagnosis and identify the underlying cause, such as tests for kidney function, autoimmune markers, or specific genetic tests.
A healthcare professional will also take a detailed medical history, ask about symptoms, and perform a physical examination to look for signs of anemia or possible causes, such as pallor, jaundice, or an enlarged spleen. The combination of blood tests and clinical assessment helps to establish a diagnosis and guide appropriate treatment.
What is the treatment for anemia?
Treatment for anemia depends on the underlying cause, severity, and type of anemia. The primary goal is to increase the hemoglobin level and red blood cell count to alleviate symptoms and improve oxygen delivery to tissues and organs. Common treatments for anemia include:
- Iron supplementation: If anemia is caused by iron deficiency, oral iron supplements are usually prescribed to restore iron levels. In some cases, intravenous iron may be necessary if oral iron is not well-tolerated or absorbed. Dietary changes to include iron-rich foods, such as red meat, poultry, fish, beans, and fortified cereals, can also help.
- Vitamin B12 and folic acid supplementation: If anemia is due to vitamin B12 or folic acid deficiency, supplementation with these vitamins is necessary to correct the deficiency and support red blood cell production. In cases of vitamin B12 deficiency caused by malabsorption or pernicious anemia, vitamin B12 injections or high-dose oral supplements may be required.
- Erythropoiesis-stimulating agents (ESAs): In some cases, such as anemia related to chronic kidney disease or cancer treatment, ESAs may be used to stimulate the bone marrow to produce more red blood cells.
- Blood transfusions: In severe cases of anemia or if the patient is experiencing significant symptoms, a blood transfusion may be necessary to quickly increase the red blood cell count and hemoglobin level.
- Treatment of underlying causes: It is essential to address the underlying cause of anemia, such as managing chronic diseases, treating infections, discontinuing medications that may contribute to anemia, or addressing other medical issues that may be contributing to the condition.
- Bone marrow or stem cell transplantation: In some cases, such as severe aplastic anemia or certain inherited disorders, a bone marrow or stem cell transplant may be considered to replace the dysfunctional bone marrow with healthy cells capable of producing red blood cells.
- Managing hemolytic anemias: For certain types of hemolytic anemias, treatments may include immunosuppressive medications, corticosteroids, or other therapies to reduce the destruction of red blood cells.
The appropriate treatment for anemia will depend on the specific situation, and a healthcare professional will develop a treatment plan tailored to the individual patient’s needs. It is essential to closely follow the recommended treatment plan and attend regular follow-up appointments to monitor the response to treatment and make any necessary adjustments.
What are the typical outcomes for anemia treatment?
The outcomes for anemia treatment depend on various factors, such as the underlying cause, severity of the anemia, the patient’s overall health, and the effectiveness of the treatment plan. In many cases, anemia can be successfully managed or even resolved with appropriate treatment.
- Iron deficiency anemia: When caused by nutritional deficiencies or other treatable conditions, iron deficiency anemia typically has a favorable outcome once iron levels are restored through supplementation and dietary changes. In most cases, hemoglobin levels and red blood cell counts return to normal, and symptoms improve.
- Vitamin B12 or folic acid deficiency anemia: With appropriate supplementation, these types of anemia can usually be corrected, and the patient’s symptoms improve. However, if vitamin B12 deficiency has led to significant neurological damage, some symptoms may persist even after treatment.
- Anemia due to chronic diseases: Managing the underlying disease often improves the associated anemia. However, the outcome depends on the severity and progression of the chronic condition. In some cases, anemia may persist despite treatment, requiring ongoing management.
- Hemolytic anemias: The outcomes for hemolytic anemias can vary widely, depending on the cause and severity. Some patients may experience a complete resolution of their anemia, while others may require ongoing treatment to manage symptoms and prevent complications.
- Inherited anemias: The outcomes for inherited anemias, such as sickle cell anemia or thalassemia, depend on the severity of the disorder and the effectiveness of the treatments available. Some patients may have a good quality of life with proper management, while others may experience significant complications and reduced life expectancy.
In general, early diagnosis and prompt treatment of anemia can improve outcomes and prevent complications. Regular follow-up with a healthcare professional is essential to monitor the response to treatment and make any necessary adjustments. In some cases, ongoing management may be necessary to maintain adequate hemoglobin levels and red blood cell counts.
What questions should I ask my doctor if I’m diagnosed with anemia?
If you are diagnosed with anemia, it’s essential to have an open and informative conversation with your doctor. Asking relevant questions can help you better understand your condition, the underlying causes, and the treatment plan. Here are some questions you may consider asking your doctor:
- What type of anemia do I have, and what is the cause?
- How severe is my anemia?
- What symptoms should I watch for, and when should I seek medical attention if my symptoms worsen?
- What tests were performed to diagnose my anemia, and are there any additional tests needed to determine the underlying cause or monitor my condition?
- What is the recommended treatment plan for my anemia, and how long will it take to see improvement in my symptoms?
- Are there any potential side effects or complications associated with the prescribed treatment?
- Will I need to take any supplements or medications, and if so, what is the appropriate dosage and duration?
- How can I adjust my diet to help manage my anemia or address any nutritional deficiencies?
- How will my anemia and treatment plan affect my daily activities or work? Are there any restrictions or precautions I should take?
- How often should I have follow-up appointments to monitor my progress and reassess my treatment plan?
- Are there any long-term effects or complications associated with my type of anemia, and what can I do to prevent or manage them?
- If my anemia is related to an underlying condition, what steps should I take to manage that condition?
Remember, your healthcare professional is there to help you manage your anemia and address any concerns you may have. Don’t hesitate to ask any additional questions that come to mind during your consultation or follow-up appointments. Understanding your condition and the recommended treatment plan is crucial for effectively managing anemia and improving your health.