What is PD-1?
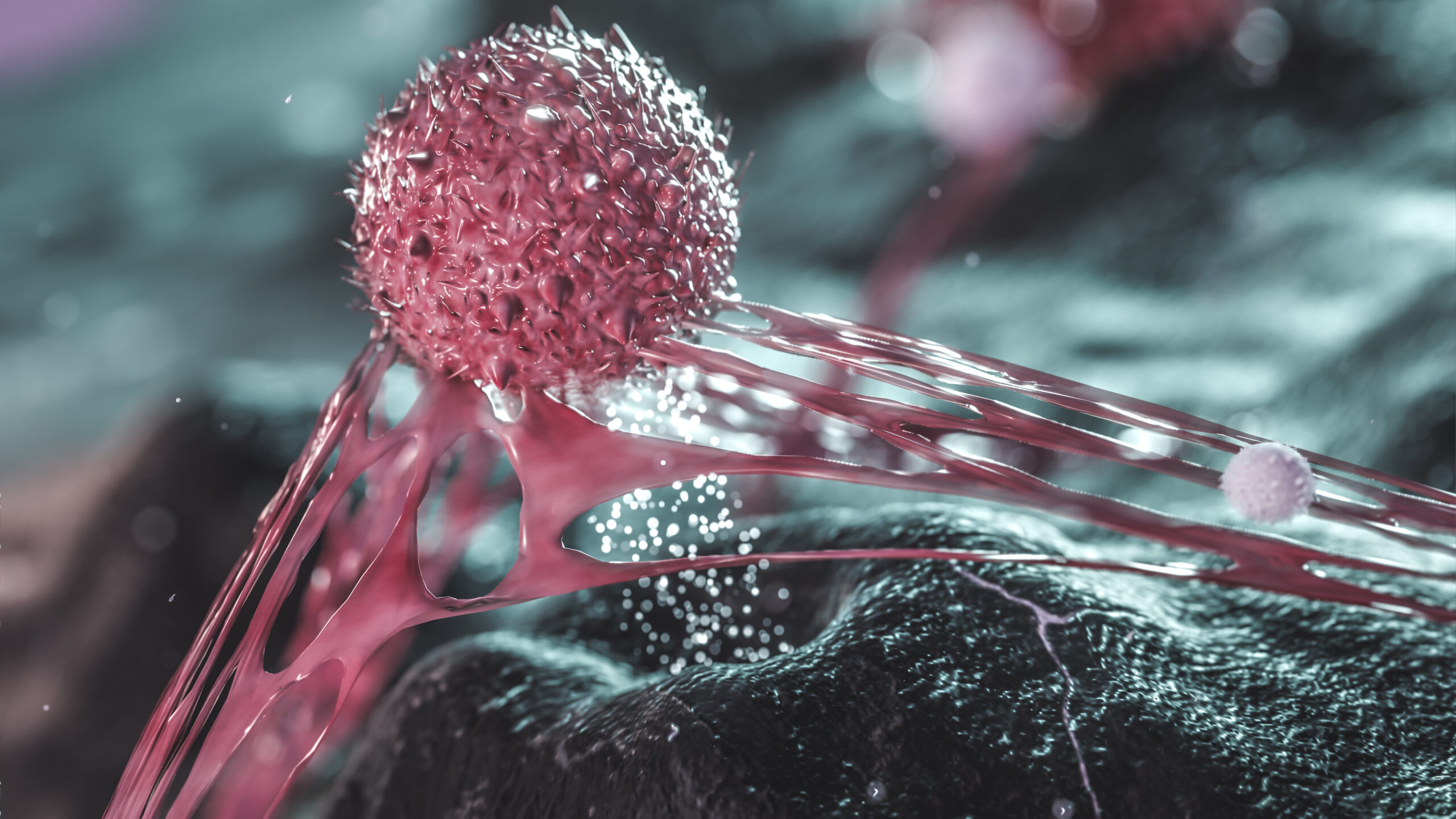
PD-1, or Programmed Death-1, is a protein receptor found on the surface of certain immune cells, particularly T cells. T cells play a crucial role in the immune system by recognizing and killing infected, damaged, or abnormal cells, including cancer cells.
The interaction between PD-1 and its ligands, such as PD-L1 (Programmed Death Ligand 1), is a critical regulatory mechanism of the immune system. When PD-L1 binds to PD-1, it sends an inhibitory signal to the T cell, which reduces the T cell’s ability to attack the cell expressing PD-L1. This mechanism helps maintain immune tolerance and prevents excessive immune responses that could damage healthy tissues.
However, some cancer cells exploit this system by overexpressing PD-L1, allowing them to evade the immune system’s attack by inhibiting T cell activity. This evasion strategy has led to the development of a class of cancer immunotherapies called immune checkpoint inhibitors, which block the interaction between PD-1 and PD-L1. By doing so, these drugs can enhance the immune system’s ability to recognize and destroy cancer cells. Immune checkpoint inhibitors, including both PD-1 and PD-L1 inhibitors, have shown promising results in treating various types of cancer.
What is PD-L1?
PD-L1, or Programmed Death Ligand 1, is a protein that plays a crucial role in the immune system’s regulation. It is found on the surface of certain cells, including some cancer cells. PD-L1 can interact with a receptor called PD-1 (Programmed Death-1) on the surface of T cells, which are immune cells responsible for recognizing and killing infected or abnormal cells, including cancer cells.
When PD-L1 binds to PD-1, it sends an inhibitory signal to the T cell, which reduces the T cell’s ability to attack the cell expressing PD-L1. As discussed above, some cancer cells exploit this system by overexpressing PD-L1, allowing them to evade the immune system’s attack.
How do PD-L1 inhibitor drugs work?
PD-L1 inhibitor drugs work by binding to PD-L1 on cancer cells, preventing it from interacting with PD-1 on T cells. By blocking this interaction, PD-L1 inhibitors help “release the brakes” on the immune system, allowing T cells to recognize and attack cancer cells more effectively. This enhances the immune system’s ability to fight cancer and can lead to better treatment outcomes for some patients with certain types of cancer.
PD-L1 inhibitors have been approved for the treatment of various cancers, including non-small cell lung cancer, bladder cancer, kidney cancer, and certain types of head and neck cancers, among others. The effectiveness of these drugs varies depending on the type of cancer and the patient’s individual response to the treatment.
What is the difference between PD-L1 and PD-1 inhibitor drugs?
PD-L1 and PD-1 inhibitors are both types of immune checkpoint inhibitors, but they target different components of the same pathway in the immune system. Here’s a brief explanation of the differences between the two:
- PD-L1 inhibitors: These drugs target the PD-L1 protein expressed on the surface of certain cells, including some cancer cells. By binding to PD-L1, these inhibitors prevent it from interacting with the PD-1 receptor on T cells (immune cells responsible for recognizing and killing infected or abnormal cells).
- PD-1 inhibitors: These drugs target the PD-1 receptor on the surface of T cells. By binding to PD-1, they prevent it from interacting with PD-L1, which is expressed on cancer cells and other cells in the immune system.
Both PD-L1 and PD-1 inhibitors work by disrupting the interaction between PD-L1 and PD-1, allowing T cells to recognize and attack cancer cells more effectively. While they target different proteins, their overall goal is the same: to enhance the immune system’s ability to fight cancer.
The choice between a PD-L1 or PD-1 inhibitor for a specific patient depends on factors such as the type and stage of cancer, the patient’s overall health, and the expression levels of PD-L1 in the tumor. In some cases, a combination of immune checkpoint inhibitors or other therapies may be used to increase treatment effectiveness.
Which PD-L1 inhibitors are currently on the market and what conditions do they treat?
While there are several PD-L1 inhibitors on the market, keep in mind that the list of available drugs and their approved indications might have changed since this article’s time of writing. Here are some of the most well-known PD-L1 inhibitors and the conditions they are used to treat:
- Atezolizumab: Used to treat various types of cancer, including non-small cell lung cancer (NSCLC), urothelial carcinoma (a type of bladder cancer), triple-negative breast cancer, and hepatocellular carcinoma (a type of liver cancer). It may be used alone or in combination with other therapies, depending on the specific cancer type and patient factors.
- Durvalumab: Approved for treating locally advanced or metastatic urothelial carcinoma (a type of bladder cancer) and unresectable stage III non-small cell lung cancer (NSCLC) after chemoradiotherapy. It may also be used in other cancer types in clinical trial settings.
- Avelumab: Used to treat metastatic Merkel cell carcinoma (a rare and aggressive type of skin cancer), metastatic urothelial carcinoma (a type of bladder cancer), and renal cell carcinoma (a type of kidney cancer) in combination with other targeted therapies.
These PD-L1 inhibitors can be used alone or in combination with other treatments, depending on the specific cancer type and patient factors. The approved indications for these drugs may continue to expand as more clinical trial data becomes available, and new PD-L1 inhibitors might enter the market over time. It is essential to consult with healthcare professionals for the most up-to-date information on available treatments and their indications.
Which PD-1 inhibitors are currently on the market and what conditions do they treat?
The other class of immune checkpoint inhibitors called PD-1 inhibitors, which target the PD-1 receptor on T cells, achieve a similar effect as PD-L1 inhibitors. Some of the PD-1 inhibitors on the market include:
- Pembrolizumab: Used to treat various types of cancer, such as melanoma, non-small cell lung cancer, head and neck squamous cell carcinoma, and others. It is often used as a first-line treatment or in combination with other therapies.
- Nivolumab: Approved for treating several cancer types, including melanoma, non-small cell lung cancer, renal cell carcinoma (kidney cancer), and Hodgkin’s lymphoma. Like pembrolizumab, it is used alone or in combination with other treatments.
New immune checkpoint inhibitors, including PD-L1 and PD-1 inhibitors, are being studied in clinical trials, and the list of approved drugs in this category may continue to expand over time. Always consult with healthcare professionals for the most up-to-date information on available treatments and their indications.
How expensive are immune checkpoint inhibitors?
Immune checkpoint inhibitors, which include PD-1 and PD-L1 inhibitors, are typically quite expensive due to the complex research and development process, as well as the manufacturing and regulatory approval costs. The exact price of these medications can vary depending on factors such as the specific drug, dosage, treatment duration, and country of purchase. Additionally, the cost of these drugs can change over time as more competitors enter the market or as patents expire.
In the United States, the cost of immune checkpoint inhibitors can range from tens of thousands to hundreds of thousands of dollars per year for a single patient. For example, a single dose of pembrolizumab can cost several thousand dollars, and patients may receive multiple doses over several months, leading to a total treatment cost that can exceed $100,000 per year. Other immune checkpoint inhibitors, like nivolumab and atezolizumab, can have similar costs.
It’s essential to note that these are the list prices, and the actual out-of-pocket costs for patients may be lower depending on factors such as insurance coverage, government assistance programs, and manufacturer-sponsored patient assistance programs. The cost of these drugs can also be quite different in other countries, depending on their healthcare systems and price regulations.
The high cost of immune checkpoint inhibitors can be a significant barrier to access for some patients, and there are ongoing discussions and efforts to find ways to lower the cost and increase the availability of these life-saving therapies.
Are immune checkpoint inhibitors safe? Do they have any side effects?
Immune checkpoint inhibitors, including PD-1 and PD-L1 inhibitors, have revolutionized cancer treatment and have shown significant benefits for many patients. However, like all medications, they can also cause side effects. These side effects occur because immune checkpoint inhibitors work by enhancing the immune system’s activity, which can sometimes lead to overactivity or attacks on healthy tissues.
Some common side effects of immune checkpoint inhibitors include:
- Fatigue
- Skin reactions such as rash, itching, or dryness
- Diarrhea or colitis
- Nausea and vomiting
- Loss of appetite
- Joint pain
- Cough or shortness of breath
In some cases, immune checkpoint inhibitors can cause more severe side effects known as immune-related adverse events (irAEs). These can affect various organs and systems in the body, including the liver, lungs, kidneys, heart, endocrine glands, and nervous system. Some examples of irAEs include:
- Hepatitis (inflammation of the liver)
- Pneumonitis (inflammation of the lungs)
- Nephritis (inflammation of the kidneys)
- Myocarditis (inflammation of the heart muscle)
- Thyroiditis (inflammation of the thyroid gland)
- Neurological complications such as Guillain-Barré syndrome or encephalitis
While these severe side effects are relatively rare, they can be life-threatening if not promptly recognized and managed. It is crucial for patients receiving immune checkpoint inhibitors to be closely monitored by their healthcare team and to report any new or worsening symptoms immediately.
Overall, immune checkpoint inhibitors are considered safe for many patients, and the benefits often outweigh the risks. However, the safety and efficacy of these drugs can vary depending on the individual patient, the specific cancer type, and the presence of other underlying health conditions. The decision to use an immune checkpoint inhibitor should always be made in consultation with a healthcare professional who can carefully weigh the potential benefits and risks for each patient.
What questions should I ask my doctor when I’m prescribed an immune checkpoint inhibitor?
When your doctor prescribes an immune checkpoint inhibitor, it’s essential to have a thorough discussion about the treatment plan, potential side effects, and expectations. Here are some questions you may want to ask your doctor:
- Why are you recommending this specific immune checkpoint inhibitor for my condition?
- What are the potential benefits of this treatment for my type and stage of cancer?
- What are the potential risks and side effects of this treatment, and how common are they?
- How can I manage or minimize these side effects, and when should I contact you if I experience any?
- Are there any alternative treatment options available, and how do they compare to the immune checkpoint inhibitor in terms of effectiveness and side effects?
- Will I need additional therapies, such as chemotherapy or radiation, in conjunction with the immune checkpoint inhibitor?
- How long will the treatment last, and how will the treatment be administered (e.g., intravenously or orally)?
- How will my progress and response to the treatment be monitored?
- Are there any restrictions or lifestyle changes I should be aware of while undergoing this treatment?
- What is the cost of the treatment, and will my insurance cover it? Are there any financial assistance programs available to help with the costs?
- Are there any ongoing clinical trials or new treatments that might be suitable for my situation?
Remember that open communication with your healthcare team is crucial for making informed decisions and managing your treatment effectively. Don’t hesitate to ask any additional questions or voice any concerns you may have during your discussion with your doctor. It’s essential to feel comfortable and well-informed about your treatment plan.